History of the Hospital Corps
The U. S. Navy Hospital Corps: A Century of Tradition, Valor, and Sacrifice
by HMCS (FMF) Mark T. Hacala, USNR
Few military organizations can look upon their histories with the same degree of pride and, in some cases awe, as can members of the Navy Hospital Corps. In its century of service, the Hospital Corps has proven itself ready to support Marines and Sailors by giving them aid whenever and wherever necessary. As the years have progressed, the tools and techniques used by Hospital Corpsmen and their forerunners have evolved, but the level of dedication has remained a strong current running through the corps’ history.
Revolutionary War
The first direction given to the organization of Navy medicine consisted of only one article in the Rules for the Regulation of the Navy of the United Colonies of North America of 1775. Article 16 stated:
“A convenient place shall be set apart for sick or hurt men, to be removed with their hammocks and bedding when the surgeon shall advise the same to be necessary: and some of the crew shall be appointed to attend to and serve them and to keep the place clean. The cooper shall make buckets with covers and cradles if necessary for their use.”
Interestingly, the cooper or barrel-maker, whose skills could be used to make bedpans, had a more detailed job description than did any kind of trained medical assistant.
A typical medical section was usually limited to two, perhaps three men: the surgeon, the surgeon’s mate, and possibly an enlisted man. The surgeon was a physician. The surgeon’s mate, usually a doctor as well, held status like that of a modern warrant officer but signed only for a particular cruise. Although usually viewed within the history of the Medical Corps, surgeon’s mates’ position and responsibilities appear more to be equivalents to senior hospital corpsmen.
Few things changed in medical techniques and organization between 1775 and 1814, the period covering America’s first naval wars. Among the less dramatic responsibilities of caring for the non-combat ill and injured was feeding and personal care of the sick. The simple daily ration of porridge or “loblolly” was sure to be carried down to those in the medical space by untrained attendants.
Surgeon’s Mate and Loblolly Boy
Congress approved an act on March 2, 1799 which copied the words of the Continental Congress’s medical department article 16 of 1775 exactly. As a result, there was still no title or job description for enlisted medical personnel. The nickname “loblolly boy” was in common use for so many years that it became the official title in Navy Regulations of 1814. The loblolly boy’s job, described in the regulations of 1818, included the following:
The surgeon shall be allowed a faithful attendant to issue, under his direction, all supplies and provisions and hospital stores, and to attend the preparation of nourishment for the sick.
The surgeon’s mates shall be particularly careful in directing the loblolly boy to keep the cockpit clean, and every article therein belonging to the Medical Department.
The surgeon shall prescribe for casual cases on the gun deck every morning at 9 o’clock, due notice having been previously given by his loblolly boy by ringing of a bell.
The U.S. Navy’s first loblolly boy of record was John Wall, who signed aboard the U.S.S. Constellation on June 1, 1798. The ship sailed with a surgeon, George Balfour, and a surgeon’s mate, Isaac Henry, as well. Eight months later, in February 1799, Capt. Thomas Truxton won a decisive victory against the French frigate L’Insurgente in the Caribbean. This would have been Loblolly Boy Wall’s first opportunity to care for shipmates wounded in battle.
Other loblolly boys who are documented in Navy records include Alexander Wood, who served aboard the U.S.S. Essex in 1802 and John Domyn aboard the frigate Philadelphia in 1803. Domyn and the rest of the crew of the Philadelphia were captured at Tripoli by Algerian pirates in October 1803 and remained captive until June 1805. Further, there was a 16 year-old loblolly boy aboard the U.S.S. Eagle, Joseph Anderson, about 1800. Anderson has the distinction of being the first known African-American loblolly boy.
Surgeon’s Steward and Loblolly Boy
A new, senior enlisted medical rate, surgeon’s steward, was introduced in the ensuing decades. The term is first seen in 1841 in Navy pay charts, but it appears that the new billet was only allowed on larger ships. By 1 April 1843, the Navy Department issued an order allowing surgeon’s steward to be assigned to brigs and schooners. The relative importance of medical Sailors was hereby increased. Surgeon’s stewards would rank second in seniority among the ship’s petty officers, next only after the master-at-arms.
Herman Melville, famed author of Moby Dick, gives a description of the surgeon’s steward aboard the frigate U.S.S. United States in White Jacket, his account of Navy life in 1843: “An official, called the surgeon’s steward, assisted by subordinates, presided over the place [sick bay]…He was always to be found at his post, by night and by day.”
Melville’s detailed description of the ship’s medical department notes that “Pills,” the surgeon’s steward’s nickname, performed a variety of duties. He assisted in preparing and passing surgical instruments during an operation. He also ran the ship’s apothecary shop, which he opened for an hour or so in the morning and in the evening. Melville remembered how he went to the steward several times when he felt a need for medicine, only to be give his freshly-ground, bitter-tasting powders in a plain tin cup. While he commented on the unpleasant taste and after-effects, Melville also noted that the potion was free of charge.
Surgeon’s Steward and Nurse
The year 1861 brought a horrible civil war to this country and, with the massive increase in the Navy, changes and developments in the medical department were sure to ensue. On 19 June 1861, a Navy Department circular order established a new name for the loblolly boy.
“In addition to a surgeon’s steward, 1 nurse would be allowed for ships with a complement of less than 200; 2 nurses would be allowed for ships with a complement of more than 200; and sufficient nurses would be allowed on receiving ships in a number proportionate to the necessities of the vessel.”
While the shipboard medical department may have only changed titles of personnel, new techniques in mass care of the sick and wounded were developed. A captured sidewheel steamer was repaired and modified to care for patients. Revisions to the ship were to include bathrooms, kitchens, laundries, even elevators and facilities to carry 300 tons of ice. On 26 December 1862, the U.S.S. Red Rover became the first Navy vessel specifically commissioned as a hospital ship. The medical complement included 30 surgeons and male nurses, as well as four nuns.
While the Civil War was often not as intense at sea services as it was for the Army, there were a number of terrible battles which necessitated a competent medical department. Pvt. Charles Brother, a Marine stationed aboard Admiral David Farragut’s flagship U.S.S. Hartford, recalls such an account in his 1864 diary. After the admiral cursed the sea mines awaiting his fleet in Mobile Bay (“Damn the torpedoes!”), Farragut directed the Hartford into the fight. Heavy Confederate fire from the Confederate ram Tennessee ensued. As would often be the case during combat action, Navy medical personnel risked becoming casualties from hostile fire. In their attempts to minister to battle casualties, medical personnel are themselves targets and sometimes do not even have the chance to render aid. Pvt. Brother noted,
The shell from the ram burst as it came through killing the Docts Stew’d [sic] instantly…Very few were slightly wounded, all were either killed instantly or horribly mangled. Our cockpit [sick bay] looked more like a slaughter house than any thing else.
Admiral Farragut’s after-action report listed a grisly count of 25 killed and 28 wounded on his ship.
Apothecary and Bayman
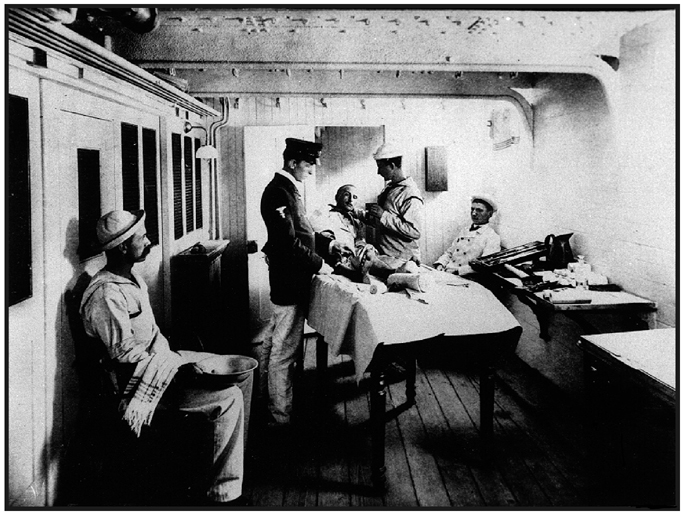 |
| An apothecary (petty officer first class) treats a shipmate aboard the USS Boston in 1888. |
Post-war reductions in the size of the Navy brought new classifications to enlisted medical personnel. The title surgeon’s steward was abolished in favor of three grades of apothecaries in 1866. Those selected as apothecaries had to be graduates of a course in pharmacy, or to possess the knowledge by practical experience. The Apothecary, First Class ranked with a warrant officer, while the second and third class were petty officer equivalents. The three rates were reduced one petty officer apothecary on 15 March 1869.
Nurse, as a title for junior enlisted medical personnel, was replace by the title “bayman,” one who manned the sick bay, in the early 1870s. U.S. Navy Regulations of 1876 used the title officially, and it remained a valid for 22 more years.
Charles Shaffer began a 50-year career in Navy medicine in 1897 as a bayman. His career path was typical for one enlisting in the medical field. Shaffer was required to enlist as a landsman (seaman apprentice), earning $16 a month. It was not until transfer to his first command that Shaffer’s rating was changed to bayman. And since the naval hospitals used civilian male nurses as opposed to baymen, Shaffer would go to a ship.
With his new title, Bayman Shaffer’s pay was upped to $18 a month. His uniform now bore two strips of piping on the cuff and a “watch mark,” a half-inch white stripe sewn around the shoulder seam of the blue jumper (blue on white uniforms) denoting him as deck force or non-engineering personnel. This stripe was worn on either the left or right shoulder seam, depending on whether the individual was assigned to the port or starboard watch. Prior to the establishment of the Hospital Corps, no specific medical insignia was worn by junior personnel.
Shaffer’s senior counterpart, the apothecary, was wearing new insignia as well, that of the newly-created (1893) chief petty officer. Its three chevrons and three arcs were surmounted by an eagle, and had a caduceus in the angle of the chevrons. An eagle whose wings extended horizontally surmounted the arcs. The rating badge described in the 1894 uniform regulations established the style which has continued, virtually unaltered, to the present day.
An apothecary of the 1890s mixed and dispensed all medication aboard ship. He was responsible for all medical department reports, supply requests, and correspondence. The apothecary administered anesthesia during surgery and would be the primary instructor for new baymen. Some of the medical skills were easily learned, though. “As a rule, baymen became skillful at bandaging,” Shaffer noted, “perhaps due to their previous training in seamanship.”
Their responsibilities did not end there, however. During shipboard surgery, the bayman focused an electric light on the incision site while the surgeon did his work on what was listed as the “combination writing and operating table”. He sterilized surgical instruments by boiling, then storing them in a solution of 5 percent phenol. Bandages and dressings were sterilized by baking them in a coffee can in the ship’s oven. Sick bay itself was prepared for surgery by wiping the entire room down with “a weak bichloride solution”. On days when the ship’s routine called for scrubbing bags and hammocks, a bayman was responsible for washing those of the sick. He assisted in the maintenance of medical department records, and had to paint the ship’s medical spaces when required.
In the last two decades of the 1800s, many in the naval medical establishment called for reforms in the enlisted components of the medical department. Medicine had by now progressed far more as a science, and civilian hospitals all had teaching schools for their nurses. Foreign navies had trained medical Sailors, and the U. S. Army had established its own Hospital Corps of enlisted men on 1 March 1887. Navy Surgeon General J. R. Tryon argued, in his annual report of 1893, against the practice of assigning landsmen to the medical department with nothing more than on-the-job-training. He advocated the urgent need for an organized hospital corps.
Physicians in the fleet were equally certain of the need for changes. Surgeon C. A. Sigfried of the U.S.S. Massachusetts made his views known in his report to the Surgeon General in 1897.
The importance of improving the medical department of our naval service is more and more apparent, in view of the recent advances in the methods and rapidity of killing and wounding. The great want is a body of trained bay men or nurses, and these should be better paid and of better stamp and fiber. Now and then we procure a good man, and proceed with his training as a bay man. He soon finds opportunity for betterment in some one of the various departments of the ship, in the matter of pay and emolument, either in some yeoman’s billet or in some place where his meager $18 per month can be suddenly increased to $30, $40, or even $60 per month. The bay man, who should be an intelligent, sober man, and well trained in many things pertaining to nursing, dieting, ambulance, and aids to wounded, and have a moderate amount of education, finds his pay at present among the lowest in the ship’s company; even the men caring for storerooms get more per month.
Hospital Corpsman: Hospital Steward and Hospital Apprentice
 |
| A hospital steward (chief petty officer) and two hospital apprentices from a ship\’s landing party medical section, 1905. |
Arguments for a professional, well-trained group of individuals to provide medical care for the Navy finally paid off. Unfortunately, it took the imminent danger of combat in the Spanish-American War to spur Congress into action. Within a bill aimed at building the armed forces was a section to provide for the Navy’s long-needed Hospital Corps. It was approved by President William McKinley on 17 June 1898. From that date to the present, either generically or by rating title, medical Sailors have been called “hospital corpsmen.”
The corps would again change the rate titles. The hospital apprentice would be the equivalent of an apprentice seaman, the hospital apprentice first class was a third class petty officer, and the hospital steward was a chief petty officer. Pharmacists were warrant officers, the first of a line of commissioned hospital corpsmen that continued until the establishment of the Medical Service Corps following World War II.
Early history of the corps set a pace of conspicuous service and involvement that would continue to the present. Before there was even a hospital corps school, Hospital Apprentice Robert Stanley was serving with the U.S. contingent at Peking. Actions by a Chinese political group that was opposed to foreign presence in China, the so-called Boxers, prompted attacks on foreign embassies in July 1900. During this action, Hospital Apprentice Stanley volunteered for the dangerous mission of running message dispatches under fire. For his bravery, Stanley became the first in a long line of hospital corpsmen to receive the Medal of Honor.
In order to ensure that the members of the new Hospital Corps were adequately trained in the disciplines pertinent to both medicine and to the Navy, a basic school for corpsmen was established at the U. S. Naval Hospital Norfolk (Portsmouth), VA. Originally called the School of Instruction, it opened 2 September 1902. Its curriculum included anatomy and physiology, bandaging, nursing, first aid, pharmacy, clerical work, and military drill. The first class of 28 corpsmen was graduated on 15 December 1902. Hospital Apprentice Max Armstrong, at the top of the alphabetical list of graduates, was naturally given his diploma first and has been heralded as the Navy’s first graduate hospital corpsman.
The school continued for a brief time and was then moved to the Naval Hospital in Washington, DC, staying in existence there until 1911. For the next three years there was no basic school for corpsmen, but the concept was revived in 1914. The next two Hospital Corps Training Schools were opened in Newport, RI and on Yerba Buena Island, CA.
Development of the Navy’s hospital corps training courses would prepare the first generation of hospital corpsmen for arduous duty, both in peace and war. A graduate of the Hospital Corps School’s sixth class, Hospital Steward William Shacklette, would find himself aboard the U.S.S. Bennington in San Diego harbor on 21 July 1905. When the ship’s boiler exploded, Shacklette was burned along with almost half the crew; the other half were killed outright. He rescued and treated numerous of his shipmates and was awarded the Medal of Honor for his bravery. Another young corpsman, Hospital Apprentice First Class William Zuiderveld of Michigan, landed at Vera Cruz, Mexico in 1914 as part of a force of Navy and Marine Corps personnel. During intense street fighting in which he was wounded himself, Zuiderveld, a graduate of the 16th class of the School of Instruction, risked his life on several occasions to aid wounded shipmates. He, too, received the Medal of Honor.
Hospital Corps: Hospital Apprentices and Pharmacist’s Mates
The next revision in the structure of the Hospital Corps would come by act of Congress on August 29, 1916. Under this plan, the rates would be hospital apprentices, second class and first class (both of whom wore a red cross on the sleeve), pharmacist’s mates, third, second, and first, and chief pharmacist’s mate. The officer contingent of the Hospital Corps would include the two warrant officer ranks of pharmacist and chief pharmacist. The reorganization would allow for a massive increase, five-fold, in the size of the Hospital Corps.
At the start of 1917 the Hospital Corps counted 1,700 men in its ranks. A concerted effort to recruit and train new personnel enabled the corps to reach its authorized strength of 3 1/2 percent of the Navy and Marine Corps, or 6,000 men. But as these plans came to fruition, the United States entered World War I in April. By the end of 1918, the corps would peak at about 17,000.
Hospital Corps: Pharmacist’s Mates in World War I
The massive war increase in Hospital Corps strength necessitated additional schools to train the newcomers. Hospital Corps School, Great Lakes, IL was established in January 1913. Wartime schools were created in Minneapolis at the University of Minnesota, in New York at Columbia University, and at the Philadelphia College of Pharmacy. A school for Naval Reserve Force hospital corpsmen was set up at Boston City Hospital. Other crash-course schools for shipboard personnel were conducted at a number of other civilian hospitals. Hospital corpsmen who were needed to serve as medical department representatives on small vessels such as destroyers were trained at the Pharmacist’s Mate School at Hampton Roads, Virginia, the forerunner of the Independent Duty Hospital Corpsman School.
Hospital corpsmen were assigned to the multitude of duty types and locations needed to support a Navy involved in a world war. Naval hospitals were opened and staffed. Ships and aircraft squadrons were given medical support. At sea, the dangers of the new war were ever present. When the troop transport USS Mount Vernon was torpedoed by a German U-boat, Pharmacist’s Mate First Class Roger Osterheld contend with over 50 casualties, over half of whom were killed.
Naval training facilities and shore establishments needed hospital corpsmen as well as did occupation forces in Haiti and other bases around the world. But World War I provided the Hospital Corps a role that would afford it some of the most gruesome and dangerous challenges it would ever face: duty with the Marine Corps.
Assignment to Marine Corps units was not completely new. Hospital corpsmen were serving with Marine occupational forces in Cuba, Haiti, and Santo Domingo at the outbreak of the war and had seen other similar service. It was the change of the Marine Corps’ role, to one of expeditionary forces in a large scale ground war, that changed what hospital corpsmen would do. Sick call and preventive medicine were continuous roles that remained unchanged. Facing artillery, mustard gas, and machine gun fire were new experiences.
Two to four hospital corpsmen were assigned to each rifle company. A first or second class petty officer would act as the company hospital corpsman and the others as platoon hospital corpsmen. In the trenches and more fixed locations, postes de secours or company aid stations were established by these contingents. A battalion aid station would have from five to seven hospital corpsmen and a chief. The senior Chief Pharmacist’s Mate and six to eight more hospital corpsmen would serve at the regimental aid station.
These hospital corpsmen lived and worked in arduous battle conditions. In one occurrence, a predawn mustard gas attack on the 6th Marines at Verdun in April 1918 had devastating consequences: 235 of the 250 in one company succumbed to the gas and had to be evacuated. The two company hospital corpsmen worked furiously to treat these patients despite their own gas injuries. One died and the other was permanently disabled. Assaults on German positions offered hospital corpsmen further chances to show their commitment. Their performance in woods well known to Marines would cause the 5th regiment’s commanding officer to write, “there were many heroes who wore the insignia of the Navy Hospital Corps at the Bois de Belleau.”
In all, some 300 hospital corpsmen, doctors, and dentists served with the 5th Marine Regiment, the 6th Marine Regiment, and the 6th Machine Gun Battalion, assigned to the Army’s 2nd Infantry Division. Their professionalism and heroism were reflected in some of the statistics they compiled. During their time in Europe, in the bloody engagements such as Meuse-Argonne and Belleau Wood, they treated over 13,000 casualties. Eighteen of their own were killed and 165 were either wounded or injured by mustard gas.
A heritage of valorous service with the Marines was born. Two hospital corpsmen received the Medal of Honor. Other decorations to hospital corpsmen included 55 Navy Crosses, 31 Army Distinguished Service Crosses, 2 Navy Distinguished Service Medals, and 237 Silver Stars. A hundred foreign personal decorations were granted to Navy hospital corpsmen, and 202 earned the right to wear the French Fourragère shoulder aiguillette permanently. Their 684 personal awards make the Hospital Corps, by one account, the most decorated American unit of World War I.
Following the war there was an inevitable decrease in the strength of the armed forces. Despite the loss of hospital corpsmen, there were still missions to perform. Nicaragua was added to the list of occupational duties to which the Marines and their hospital corpsmen were assigned in 1927. Ships and naval hospitals still required Hospital Corps staff. Dedicated members of the Hospital Corps remained in the service, doing what they loved, despite the lack of advancement opportunity. In the years between the wars, time in rate from pharmacist’s mate second class to pharmacist’s mate first class was 8 years.
Hospital Corps: Pharmacist’s Mates in World War II
 |
| Women entered the Hospital Corps in World War II as WAVES. |
World War II became the period of Hospital Corps’ greatest manpower, diversity of duty, and instance of sacrifice. Between 1941 and 1945, the ranks of this small organization swelled from its pre-war levels of near 4,000 to over 132,000 personnel. This increase came to fulfill new responsibilities with new technologies at new duty stations. In the face of great adversity, the Hospital Corps would cement its reputation for effectiveness and bravery.
The Navy’s fleet expanded to thousands of ships and the Marine Corps grew from a few regiments to six divisions. A two ocean war produced horrific numbers of casualties. The Hospital Corps would have to grow to meet the needs of casualty collection, treatment, and convalescence. To educate the influx of new Sailors, Hospital Corps Training School at Portsmouth, VA was augmented by a temporary school at Naval Hospital Brooklyn, NY. The school at Great Lakes was recreated in 1942, and others were started at Farragut, ID and at Bainbridge, MD in 1943. A separate Hospital Corps Training School was established for women at Bethesda, MD in January, 1944. Specialized schools were opened to train pharmacist’s mates for independent duty and for service with the Marines. Additionally, courses were established to instruct personnel on new equipment and techniques in dozens of developing medical fields.
Shore-based duty sent Hospital Corps personnel to hospitals and dispensaries in the United States and abroad. Advance base hospitals on newly-captured Pacific islands formed a crucial link in the chain of evacuation from battle sites. Those facilities in Hawaii or England received casualties from their respective fronts. Stateside hospitals watched over wounded service personnel as their recuperation continued. Hospital corpsmen made the treatment of American casualties possible at each of these by providing technical support and direct patient care.
Duty on surface ships afforded hospital corpsmen numerous challenges and abundant environments in which to face them. Hospital ships required the services of personnel in much the same way as shore-based hospitals, except that those on ship were afloat and subject to attack. Other classes of vessels, such as landing ships, tank (LSTs) and patrol craft, escort and rescue (PCERs) became large floating clinic/ambulances which required additional Hospital Corps personnel.
Combatant ships and transports in the Atlantic, Pacific, and Mediterranean theaters took casualties from ships, aircraft, and submarines throughout the war, necessitating the service of well-trained hospital corpsmen. Casualties could be staggering on attacked ships. In one example, the aircraft carrier USS Bunker Hill sustained 392 killed and 264 wounded when it was hit by two kamikazes.
Role of submarine hospital corpsmen developed into one of great importance. Hospital corpsmen treated 549 survivors of air or sea calamities, U.S. and enemy alike. In one case, three Sailors were seriously wounded, the submarine’s C.O. wrote, “the chief pharmacist’s mate is particularly commended for his quick and efficient action in caring for these three wounded shipmates…He has been recommended for promotion and the Bronze Star Medal.”
The most dramatic accomplishments of submarine hospital corpsmen were three who had to do surgery while submerged. Pharmacist’s Mate First Class Wheeler “Johnny” Lipes performed a successful appendectomy aboard the USS Seadragon on 11 September 1942. Lipes, who had been a surgical technician, used improvised instruments made from mess deck utensils and instructed assistants as the procedure went on in the officers’ wardroom. PhM1c Harry Roby performed the same act on the USS Grayback as did PhM1c Thomas Moore aboard USS Silversides, both in December 1942.
Approximately 300 hospital corpsmen sat out all but the early days of the war when they were captured by the Japanese who invaded the Philippines. In prisoner of war camps and huddled in POW “hell ships”, they endured malnutrition, disease, torture, and brutality. One hundred thirty-two hospital corpsmen died as prisoners during World War II, a death rate almost 20 percent higher than among other American POWs.
Hospital corpsmen served on the beaches not only in the island campaigns of the Pacific, but in Europe as well. Teams of Navy medical personnel formed aid stations with beach battalions at Sicily and Normandy, treating Army and allied wounded under fire. Hospital corpsmen ensured the survival of these casualties until they could reach hospitals in England.
Of all the hospital corpsmen in World War II, Fleet Marine Force personnel endured, perhaps, the most grueling side of war. As they swarmed numerous beaches in the Pacific, they became targets themselves as they braved fire to reach downed comrades. At Guadalcanal, Tarawa, Peleliu, Saipan, Tinian, Kwajalein, Iwo Jima, and Okinawa, hospital corpsmen bled and died, often in greater numbers than the Marines for whom they cared. Hospital Corps casualties in the 4th Marine Division at Iwo Jima, for example, were 38 percent.
Pharmacist’s Mate First Class Ray Crowder made notes of his combat experiences in his diary:
Most of the men who had been wounded previously were hit again…I was hit by a piece of shrapnel in my leg but I overlooked it until later. As soon as I could get my wits together…I began to do what I could for the guys. Two of the men were screaming with shock. Darkness had already fallen and I couldn’t see what I was doing. All that I could do was to feel the blood and try to get a pressure bandage put over it to stop the bleeding.
Pharmacist’s Mate Second Class John H. Bradley’s heroism with the 28th Marines on Iwo Jima is typical of acts repeated by hospital corpsmen throughout the war. On seeing a wounded Marine, Bradley rushed to his aid through a mortar barrage and heavy machine gun fire. Although other men from his unit were willing to help him with the casualty, Bradley motioned them to stay back. Shielding the Marine with his own body, the hospital corpsman administered a unit of plasma and bandaged his wounds. Through the gunfire, he then pulled the casualty 30 yards to safety.
PhM2c Bradley was awarded the Navy Cross for his valor, but he is not usually remembered for this act. Days later, he and five Marines were captured in Joe Rosenthal’s photograph of the second flag raising on Mt. Suribachi. The image was reproduced more than perhaps any photo in history. It was the theme for the Marine Corps War Memorial in Arlington, VA and made Bradley the first U.S. Navy Sailor to appear on a postage stamp. His likeness as a dedicated American serviceman is the most famous in the Hospital Corps’ history.
Members of the Hospital Corps treated some 150,000 combat casualties during the war. This does not include thousands of others, those plagued by disease and injured in the line of duty, who were aided by their medical shipmates. The cost of this service was high: 1,170 hospital corpsmen were killed in action and thousands more were wounded. But their valor in doing their jobs was great. Hospital corpsmen earned 7 Medals of Honor, almost half of those awarded to Sailors in the war. In addition, they earned 66 Navy Crosses, 465 Silver Star Medals, and 982 Bronze Star Medals.
A New Hospital Corps:
Massive reorganization of the armed forces took place after World War II. A new Department of Defense was established, and the Army-Navy Medical Service Corps Act removed commissioned allied health and medical administration officers from the Hospital Corps. This law also provided for a separate Dental Technician rating, which remained a component of the Hospital Corps until 1972. Women in the Hospital Corps had previously been WAVES, or members of the Women’s Reserve, U.S. Naval Reserve. New legislation permitted women to enlist in the Regular Navy, and HM1 Ruth Flora became the first hospital corpsman to do so on 12 July 1948
Effective 2 April 1948 the Navy changed the names and insignia of the Hospital Corps. The new titles were hospital recruit, hospital apprentice, hospitalman, hospital corpsmen third, second, and first class, and chief hospital corpsman. The red Geneva cross, which had marked corpsmen for 50 years, was replaced in the rating badge with the original mark of the winged caduceus. The rates of senior chief and master chief hospital corpsman were added in 1958.
Hospital Corpsmen in Korea:
As part of a United Nations force, Marines were committed to the Korean peninsula when South Korea was invaded by its northern neighbor in the summer of 1950. Within the first year, hospital corpsmen had participated in the dramatic landing at Inchon and the frigid retreat from the Chosin Reservoir. By the summer of 1951, a stalemated line of opposing forces took static positions. For the next two years, the war would be reminiscent of World War I, with bunkers, trenches, raids and artillery fire. The slow war of attrition was nonetheless lethal. In late March 1953, 3,500 Chinese Communist Forces soldiers attacked three outposts–Reno, Vegas, and Carson–of 40 Marines and one hospital corpsmen each. Out of this fighting came two Medals of Honor and numerous other decorations. In the Nevada Cities Outpost battles, most of the hospital corpsmen who were involved at the small unit level were either killed or wounded.
Although only one Marine division was involved in the war, the Hospital Corps lost 108 killed in action. Disproportionate to their numbers was their heroism. In Korea, hospital corpsmen earned 281 Bronze Star Medals, 113 Silver Star Medals, and 23 Navy Crosses. All five enlisted Navy Medals of Honor were awarded to Navy Hospital Corpsmen serving with the Marines.
Hospital Corpsmen in Vietnam
American military commitment in Southeast Asia grew in the decades following World War II. As early as 1959, a few hospital corpsmen provided medical support for U. S. military personnel as part of the American Dispensary at the U.S. Embassy. Four years later, in 1963, Navy Station Hospital, Saigon was created. Ninety hospital corpsmen would staff the facility, which provided care for U. S. and allied (Australian, New Zealand, Filipino, and South Korean) military, as well as South Vietnamese civilians. These medical personnel conducted routine medical care and treated the victims of combat and terrorist actions until the hospital was transferred to the Army in 1966.
A new hospital was constructed in 1965 at Naval Support Activity Da Nang. A staff of 485 hospital corpsmen worked with doctors and nurses to care for combat casualties. The hospital, which was designed primarily to care for Marines in the I Corps sector, treated 23,467 patients in 1968 alone. Although not on the front lines, the hospital corpsmen here were subjected to routine rocket and mortar attacks.
Hospital corpsmen were assigned aboard ships of various kinds, providing off-shore medical support to U. S. forces. The largest commitment here was on the hospital ships USS Repose and USS Sanctuary. Some 200 hospital corpsmen, representing the gamut of technical specialties, worked on each ship. Teams of 20 hospital corpsmen served on LPH class amphibious ships. Others supported the riverine force on APB class base ships.
U. S. State Department initiatives and the Medical Civic Action Program (MEDCAP) provided medical support for Vietnamese civilians. Beyond routine aid and treatment, the hospital corpsmen working through these programs provided guidance in sanitation and preventive medicine throughout South Vietnam.
By far the Hospital Corps’ largest contribution in Vietnam was with Marine Corps units. Starting with the 50 who landed with the Marines at Da Nang in 1965, the enlisted medical component would grow to 2,700 hospital corpsmen assigned to 1st and 3d Marine Divisions, 1st Marine Air Wing, and other combat support units. Two medical battalions and two hospital companies operated field hospitals, collecting and clearing units, and dispensaries which treated the flow of combat casualties from the field. Closer support was provided at the battalion aid station (BAS) level, where casualties could be stabilized before evacuation to more definitive care. The BAS was often bypassed because of the exceptional medical evacuation capabilities of helicopter medical evacuation (MEDEVAC).
The most dangerous role of the hospital corpsman in Vietnam was in the field. Special units, such as Navy SEAL teams and Marine reconnaissance units took medical Sailors with them, as did the artillery, air, and infantry elements of the Marine Corps. Most of the 53 hospital corpsmen assigned to an infantry battalion served with rifle companies, one or two men per platoon of about 40. These Sailors patrolled with their Marines, risked the same dangers, and rendered the aid that saved the lives of thousands.
Contributions of hospital corpsmen in Vietnam were noteworthy, as they cared for over 70,000 combat Navy and Marine Corps combat casualties and countless military and civilian sick call patients. Their valor was great. HM3 Donald E. Ballard, HM3 Wayne M. Caron, and HM2 David R. Ray earned the Medal of Honor for heroism. HM3 Robert R. Ingram received his Medal of Honor for Vietnam in 1998. Additionally, 30 hospital corpsmen received the Navy Cross, 127 the Silver Star Medal, and 290 the Bronze Star Medal. The names of 638 hospital corpsmen were killed in action there, more than in any other war except World War II. Too many more–4,563–would earn the Purple Heart.
HM2 Chris Pyle wrote the following letter home before assignment with 1st Marine Division in Vietnam.
Many people have died to save another. The Navy Corpsman has had more honors bestowed on him than any other group. My life has but one meaning, to save or help someone. Soon I will be going over to Vietnam. I have my fears and beliefs, but they lay hidden under my emotions. That’s why God has made me so. Someday I will see before me a wounded marine. I will think of all kinds of things, but my training has prepared me for this moment. I really doubt if I will be a hero, but to that Marine I will be God. I am hoping that no one will die while I am helping him; if so, some of myself will die with him. Love for fellow man is great in my book. It’s true they make me mad at times but no matter who it is, if he’s wounded in the middle of a rice paddy, you can bet your bottom dollar that whatever God gave me for power, I will try until my life is taken to help save him, and any other.
Five months later, on 28 May 1969, HM2 Pyle was killed in action.
Hospital Corpsmen in Beirut
A different part of the world would beckon hospital corpsmen in the 1980s, southwest Asia. The objective was a “peacekeeping” mission in Beirut, Lebanon, in which U.S. forces participated with those of France, Italy, and the Great Britain in a Multinational Force. Here, hospital corpsmen from the ships of a Mediterranean Amphibious Ready Group and a Marine Amphibious Unit were assigned to stop a bloody, eight-year old factional civil war. By the end of August, 1983, the peacekeepers had become targets and responded in a ground war that was all but unknown back in the U.S.
Firefights at isolated outposts soon produced casualties, and hospital corpsmen responded under fire to treat their wounded Marines. When a mortar round hit one of the Marine positions, one hospital corpsman, HN Victor Oglesby, found himself with five wounded Marines, his platoon sergeant dead, and his platoon commander barely alive. Two months later, on 23 October a uniformed suicide truck bomber attacked the headquarters of 1st Battalion, 8th Marines. The truck bomb unleashed the largest non-nuclear blast ever detonated, and killed 241 Americans. Almost the entire battalion aid station–15 hospital corpsmen and the battalion surgeon–were killed. The casualty count for the Hospital Corps would be the next costly after World War I. One of the three hospital corpsmen who survived the blast, HM3 Donald Howell, tended to wounded Marines while trapped in the rubble and wounded himself. The relief unit for the 24th Marine Amphibious Unit would not arrive in Lebanon until they had invaded the small Caribbean nation of Grenada.
Hospital Corpsmen in the Persian Gulf War
The 1990-91 Iraqi invasion of Kuwait gained a strong response from the U.S. and the world. Preparations were made to drive the Iraqi Army out of the tiny country, and corpsmen were readied to respond to the needs of their shipmates. Hospital corpsmen around the globe reacted, as their ships, stations, and Marines deployed or prepared to receive casualties. In fact, the first Navy casualty of the war was a hospital corpsman. Of the vast number of Naval Reservists called to active duty, the largest single group activated was hospital corpsmen. Of an inventory of just over 12,000 hospital corpsmen in the Naval Reserve, 6,739 were recalled to active duty. The largest group of them, 4,617, served at medical treatment facilities and casualty receiving centers. 1,142 went to Marine Corps units, 841 to Fleet Hospitals 6 and 15, 471 of them were assigned to the hospital ships Mercy and the Comfort.
Hospital Corpsmen in Somalia
U.S. forces would again try to bring stability to a troubled land: Somalia. Hospital corpsmen there faced both bullets and the needs of a starving populace. One, HM3 Timothy E. Quinn, wrote a letter describing his experiences in February 1993. “I was on a foot patrol that got pinned down by automatic weapons fire, and here I am tucked up against a tree trying to get small…” He continued, “I go out to orphanages and do simple sick call and such…the people there tell us that food is now plentiful, and that no one is dying of hunger anymore, but now the medical problems are much more apparent.”
Hospital Corpsmen Today
In its first century, the Hospital Corps has compiled a truly honorable legacy of valor and sacrifice. In addition to the wars and conflicts recounted here, hospital corpsmen have responded to natural disasters, military accidents, and other peacetime emergencies. Moreover, they have maintained the regular health of their Sailors and Marines, giving immunizations, conducting preventive medicine efforts, and holding sick call. Today, the 23,000 regular and 6,000 reserve members of the Navy Hospital Corps continue to serve around the globe. They are assigned to naval hospitals and clinics, to surface ships and submarines. They fly search and rescue missions and deploy with Seabees. They maintain constant battle readiness with Marine Corps units and SEAL teams.
Hospital corpsmen have always had the job of maintaining the health of their shipmates. Their innumerable instances of heroism, of consciously exposing themselves to danger to save lives, are not spectacular because they were required to act. Their displays of courage have been noteworthy because these men and women cared about their shipmates.






